Did you know? The Global Diagnostic Biomarkers Market is projected to attain a value of USD 715.25 billion by 2035 at a CAGR of 19.75% during the forecast period 2025-2035, reflecting the rapidly growing recognition of their clinical importance.
The surge in diagnostic biomarkers adoption stems from their ability to provide objective, measurable indicators of biological processes, pathological conditions, or therapeutic responses.
From cancer detection to neurological disorders, these molecular tools enable clinicians to make informed decisions based on individual patient profiles rather than broad population averages.
Advanced technologies like RNA sequencing have further accelerated biomarker discovery, revealing previously hidden patterns in gene expression that correlate with disease states and treatment outcomes.
In this article, we explore the comprehensive landscape of diagnostic biomarkers, examining their mechanisms, applications, and the technological innovations that continue to expand their clinical utility in modern healthcare.
Key Takeaways
- Diagnostic biomarkers serve as measurable indicators of disease states, enabling early detection and personalized treatment approaches across multiple medical specialties, from oncology to cardiology.
- RNA sequencing technologies have revolutionized biomarker discovery by providing comprehensive transcriptome analysis, revealing novel gene expression patterns that correlate with disease progression and treatment response.
- Advanced AI-driven platforms are streamlining biomarker identification and interpretation, reducing the time from discovery to clinical application while improving accuracy and accessibility for researchers and clinicians.
- Despite significant progress, challenges remain in standardization, cost-effectiveness, and biological variability, requiring continued innovation in analytical platforms and regulatory frameworks.
What are Biomarkers?
Biomarkers are measurable biological indicators that help detect, track, or predict the progression of diseases. These can include proteins, nucleic acids, metabolites, and other cellular components found in blood, tissue, urine, or saliva.
Ideally, it should be:
- Specific to the target condition.
- Detectable by minimally invasive sampling.
- Quantifiable with reproducible assays.
- Clinically actionable (guides therapy, triage, or prognosis)
Unlike symptom-based diagnoses, biomarkers provide objective data that can detect diseases before symptoms appear.
Understanding the distinct characteristics that make certain biological molecules effective diagnostic biomarkers requires examining the various categories and types available to researchers and clinicians today.
Types of Diagnostic Biomarkers
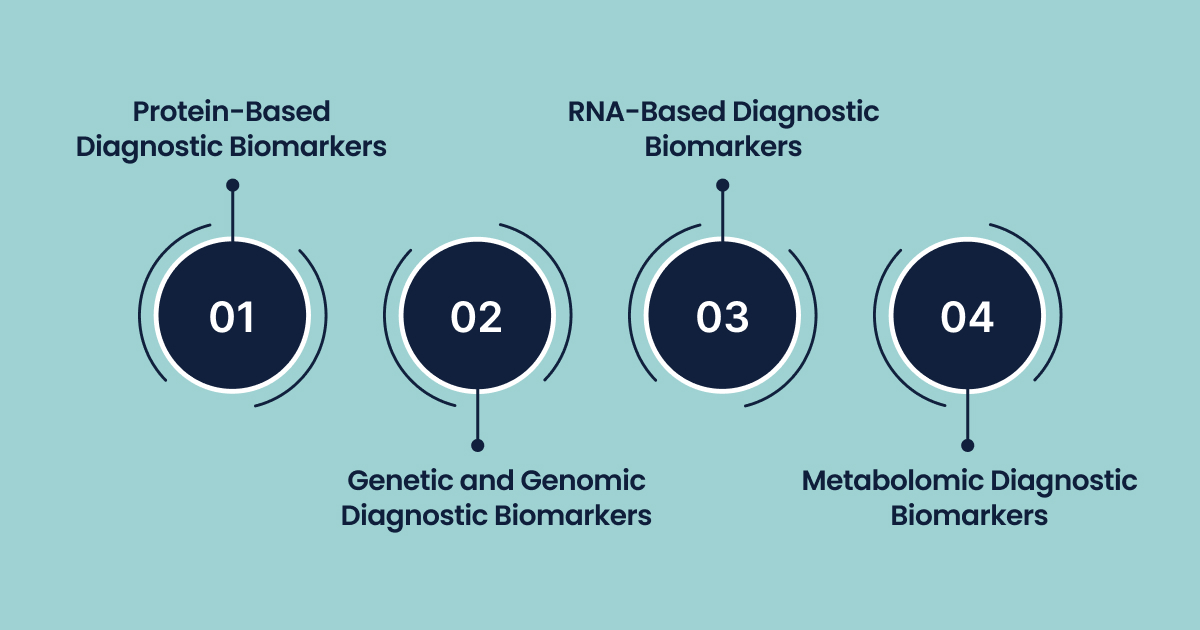
The classification of diagnostic biomarkers encompasses several distinct categories, each offering unique advantages for specific clinical applications and research objectives.
Protein-Based Diagnostic Biomarkers
Protein biomarkers represent the most established category in clinical diagnostics.
- These markers reflect the functional output of cellular processes and often correlate directly with disease severity and progression.
- For example,
- C-reactive protein (CRP) levels can indicate inflammation
- Prostate-specific antigen (PSA) levels are used to diagnose and monitor prostate cancer.
Recent advances in proteomics have enabled the identification of novel protein signatures, such as the discovery of PHGDH protein biomarkers for tissue-specific diagnostics. This is expanding the repertoire of available protein-based diagnostic tools.
Genetic and Genomic Diagnostic Biomarkers
These are DNA-based biomarkers that focus on genetic variations, mutations, and chromosomal aberrations that predispose individuals to specific diseases or influence treatment responses.
- Examples include
- BRCA1 and BRCA2 mutations for hereditary breast cancer risk assessment
- Microsatellite instability markers for colorectal cancer diagnosis.
These genetic markers provide stable, inherited information that remains constant throughout an individual’s lifetime, making them particularly valuable for risk assessment and personalized treatment planning.
RNA-Based Diagnostic Biomarkers
Transcriptomic biomarkers analyze gene expression patterns to provide dynamic insights into cellular activity and disease states.
- Examples include
- Specific microRNA signatures for cancer classification
- Long non-coding RNA patterns for neurological disorder diagnosis.
- Unlike genetic markers, RNA biomarkers reflect real-time cellular responses to environmental factors, disease progression, and therapeutic interventions.
- RNA-seq can detect both early mutations and high-molecular-risk mutations.
Thus it can discover novel cancer biomarkers and potential therapeutic targets, monitor diseases, and guide targeted therapy.
Metabolomic Diagnostic Biomarkers
Metabolite-based biomarkers represent the end products of cellular biochemical processes, providing insights into metabolic pathway alterations associated with disease states.
- These small-molecule markers, including amino acids, lipids, and organic acids, offer rapid, cost-effective diagnostic opportunities.
- Examples include
- Glucose levels for diabetes diagnosis.
- Specific metabolic signatures for inborn errors of metabolism.
The integration of these diverse biomarker types creates comprehensive diagnostic panels that leverage the strengths of each category. This approach compensates for individual limitations, leading to more robust and reliable diagnostic methods.
Mechanisms of Action of Diagnostic Biomarkers
The effectiveness of diagnostic biomarkers stems from their ability to reflect underlying biological processes through specific molecular mechanisms that can be measured and interpreted clinically.
Molecular Expression Pathways
Diagnostic biomarkers function by altering normal molecular expression patterns that occur during disease development and progression.
- At the cellular level, pathological conditions trigger cascade reactions that modify protein synthesis, gene expression, and metabolic pathway activity.
- These changes manifest as measurable differences in biomarker concentrations or patterns compared to healthy baseline levels.
- RNA-based diagnostic biomarkers exemplify this mechanism through their ability to capture real-time transcriptional changes.
- When cells encounter disease-related stress, infection, or malignant transformation, specific genes become upregulated or downregulated in predictable patterns.
These expression changes can be detected through advanced sequencing technologies that quantify thousands of transcripts simultaneously, revealing disease-specific signatures that serve as diagnostic indicators.
Signal Transduction and Pathway Disruption
Disease states often disrupt normal cellular signaling pathways. This involves creating detectable biomarker signatures through altered protein phosphorylation, metabolite accumulation, or modified enzyme activity.
- For example, oncogenes and tumor suppressor genes create distinct expression profiles when activated or inactivated during cancer development.
- Here, fusion genes have been identified as therapeutic targets in acute myeloid leukemia.
- Recurrent gene fusions, which drive cancer, show how pathway disruptions create actionable biomarker targets.
Inflammatory and Immune Response Mechanisms
Many diagnostic biomarkers reflect the body’s inflammatory and immune responses to pathological conditions.
- Cytokine expression patterns, inflammatory protein levels, and immune cell activation markers provide insights into disease activity and progression.
- These mechanisms are particularly relevant for autoimmune disorders, infectious diseases, and cancer, where immune system dysregulation creates measurable biomarker signatures.
Epigenetic Regulation Mechanisms
Epigenetic modifications, including DNA methylation and histone modifications, create stable biomarker patterns that persist throughout disease progression.
These mechanisms allow diagnostic biomarkers to capture long-term cellular changes that may not be reflected in immediate gene expression or protein levels, providing complementary diagnostic information.
Understanding these fundamental mechanisms enables researchers and clinicians to select appropriate biomarkers for specific diagnostic applications and interpret results within the proper biological context.
This ultimately leads to more accurate and meaningful diagnostic outcomes.
Applications of Diagnostic Biomarkers
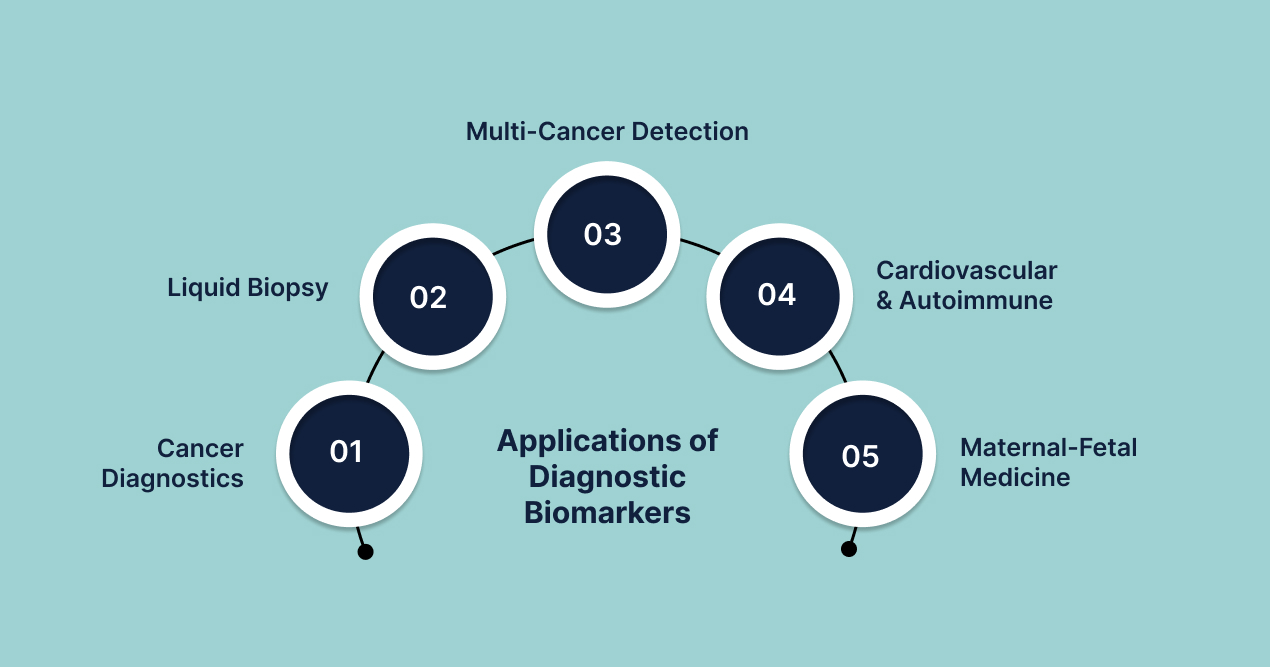
The clinical applications of diagnostic biomarkers span multiple medical specialties, providing transformative capabilities for disease detection, monitoring, and management across diverse healthcare settings.
- Oncology and Cancer Diagnostics
Cancer diagnosis and management represent the most developed application area for diagnostic biomarkers, with numerous FDA-approved markers guiding clinical decisions.
ctDNA & Liquid Biopsy Revolution
Cell-free circulating tumor DNA (ctDNA) detects somatic mutations, methylation changes, and fragmentomics patterns. Clinical uses include:
- Screening high-risk populations.
- Determining minimal residual disease (MRD).
- Real-time resistance mutation tracking.
Multi-Cancer Early Detection (MCED) Blood Tests
Galleri doubled cancers found beyond standard screening, with 88% accuracy in predicting the tissue of origin. The U.K. NHS-Galleri trial (140,000 participants) will report stage-shift data in 2026.
- PAC-MANN protease assay flagged pancreatic ductal adenocarcinoma with 85% accuracy in a 2025 OHSU study.
- A 5-protein early-PDAC signature (TIMP1 + ICAM1 + THBS1 + CTSD + CA19-9) reached 85% sensitivity at 98% specificity in high-risk cohorts.
Angelina Jolie’s 2013 op-ed on her BRCA1 result triggered a 90% surge in genetic referrals and a sustained rise in prophylactic mastectomies. Her story illustrates how powerful public narratives accelerate genetic-biomarker uptake.
| Test | Core Technology | Cancers Detected | Sensitivity (all stages) | Specificity | Regulatory Status |
| Galleri | cfDNA targeted methylation sequencing | >50 | 51.5% | 99.5% | Commercial LDT; NHS trial |
| Galleri (PATHFINDER-2) | Same | Same | PPV 43% → higher in update | 99.5% | Registration trial |
These approaches combine protein markers, genetic mutations, and epigenetic modifications to achieve high sensitivity and specificity for early-stage disease detection, potentially revolutionizing cancer screening programs.
- Cardiovascular Disease Applications
Cardiovascular diagnostic biomarkers have evolved beyond traditional markers like troponin and B-type natriuretic peptide to include comprehensive RNA signatures that predict heart failure risk, treatment response, and prognosis.
- High-sensitivity cardiac troponin (hs-cTn) assays identify myocardial injury within <1 h.
- A 2023 Spanish multicenter ED study showed AUC > 0.9 and cut time-to-decision by 50%.
- Incorporation into an updated HEART pathway improved AMI detection and reduced unnecessary admissions.
High-sensitivity assays enable earlier detection of myocardial injury, while novel biomarkers like galectin-3 and ST2 provide insights into heart failure progression and therapeutic monitoring.
- Gastroenterology & Autoimmunity
Gastroenterologists utilize fecal calprotectin testing. Fecal calprotectin (FC) is a protein primarily found in the cytoplasm of neutrophils, a type of white blood cell involved in inflammatory responses.
- When there is inflammation in the gastrointestinal (GI) tract, neutrophils migrate to the inflamed area and release calprotectin, which can then be measured in stool samples.
- Fecal calprotectin distinguishes between inflammatory bowel disease (IBD) and functional disorders with 88% sensitivity and 80% specificity.
- Cut-offs of >50 µg/g guide colonoscopy triage. Real-world audits report 118 fewer colonoscopies after calprotectin-based algorithms.
The tennis champion Venus Williams’ withdrawal from the 2011 U.S. Open spotlighted Sjögren’s syndrome diagnosis, spurring subsequent biomarker research. This led to Augusta University’s patented salivary panel for the early detection of autoimmune diseases.
- Maternal-Fetal Medicine Revolution Through Non-Invasive Testing
Obstetricians routinely employ cell-free DNA-based non-invasive prenatal testing (NIPT). NIPT analyzes cell-free fetal DNA (cfDNA) circulating in the mother’s bloodstream.
This cfDNA originates from the placenta and reflects fetal genetic material, offering a safer method to screen for chromosomal abnormalities such as Down syndrome.
- Detects trisomy 21 with 99.7% sensitivity and 0.04% false-positive rate.
- Global 60% decline in invasive amniocentesis after NIPT rollout.
The potential of NIPT is rapidly expanding beyond its initial scope, with a growing focus on the detection of single-gene disorders, especially those arising from de novo or paternally inherited variants.
This advancement, particularly through whole-exome sequencing of cfDNA, represents the next frontier in prenatal screening.
- Neurological and Psychiatric Disorders
Neurological applications of diagnostic biomarkers focus on conditions like Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis, where early detection significantly impacts treatment outcomes.
- Clinical researchers validated plasma p-tau217 as a breakthrough biomarker that detects amyloid and tau pathology with 91% accuracy in a 1,213-patient Swedish multicenter trial.
- Genetic counselors report that individuals carrying two APOE4 copies face 8-10 times higher Alzheimer’s risk, driving demand for risk stratification services.
Chris Hemsworth‘s public disclosure of his double-APOE4 genotype in 2022 sparked global interest in preventive biomarker testing.
- Also, Researchers developed the α-synuclein Seed Amplification Assay (αSyn-SAA), which confirms Parkinson’s pathology in 93% of clinical cases with 96% specificity.
- This revolutionary test detects prodromal disease before motor symptoms appear, while the FDA issued a 2024 “Letter of Support” encouraging its use in clinical trials.
Cerebrospinal fluid and blood-based biomarkers now enable the detection of Alzheimer’s pathology decades before symptom onset, facilitating early intervention strategies and clinical trial enrollment.
Similarly, RNA biomarkers for psychiatric conditions are emerging as tools for diagnosis, treatment selection, and monitoring therapeutic responses in depression, schizophrenia, and bipolar disorder.
Comprehensive Clinical Performance Analysis of Biomarkers
| Disease Category | Primary Biomarker | Sample Type | Sensitivity | Specificity | Clinical Readiness | Latest Breakthrough |
| Multi-Cancer | Methylation signatures (Galleri) | Plasma | 51.5% | 99.5% | Commercial LDT | PATHFINDER-2 results (2023) |
| Pancreatic Cancer | PAC-MANN protease panel | Plasma | 85% | 92% | Magnetic nanosensor POC | OHSU validation (2025) |
| Alzheimer’s Disease | Plasma p-tau217 | Blood | 91% | 87% | CLIA launch planned for 2025 | Swedish multicenter trial (2024) |
| Parkinson’s Disease | αSyn-SAA | CSF | 93% | 96% | Research-grade | FDA Letter of Support (2023) |
| Acute MI | High-sensitivity troponin | Whole blood | >90% AUC | 95% | Handheld POCT devices | Spanish ED study (2023) |
| Prenatal Screening | cfDNA NIPT | Maternal plasma | 99.7% | 99.9% | Standard of care | Global implementation (2024) |
| IBD | Fecal calprotectin | Stool | 88% | 80% | At-home ELISA kits | Clinical algorithm validation (2024) |
The expanding applications of diagnostic biomarkers continue to create new opportunities for improved patient care across virtually every medical specialty, driven by advancing technologies and a growing understanding of disease biology at the molecular level.
Technologies for Biomarker Identification
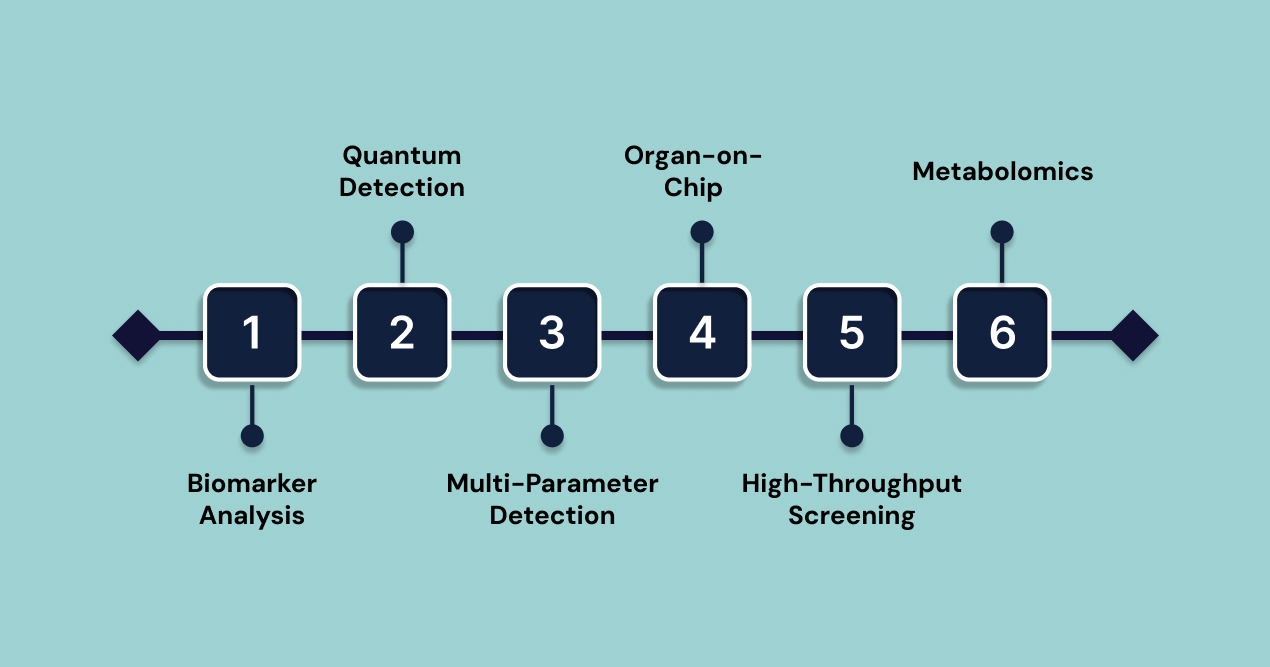
The discovery and validation of diagnostic biomarkers rely on advanced technologies capable of detecting and analyzing complex biological signatures with high precision.
- Circulating Biomarker Analysis
Liquid biopsy technologies revolutionize cancer diagnostics by analyzing circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), and other biomarkers. These technologies support early detection, staging, prognosis evaluation, and real-time tumor monitoring. The global liquid biopsy market is projected to grow from $6.39 billion in 2025 to $25.43 billion by 2035.
- Quantum-Enhanced Detection
Quantum sensors, including nitrogen vacancy centers in diamond crystals, provide ultrasensitive biomarker detection with minimal sample volume. Quantum dot-based biosensors exploit unique optical properties for precise detection of DNA, microRNAs, proteins, and cells, offering a high level of sensitivity.
- Multi-Parameter Detection
Advanced biosensors enable simultaneous detection of multiple biomarkers using electrochemical, optical, and surface plasmon resonance approaches. Field-effect transistor-based biosensors, combined with 2D materials like graphene, enhance detection sensitivity. Terahertz metamaterial biosensors provide 100-fold sensitivity improvements and are integrated with microfluidics for enhanced performance.
- Microphysiological Systems
Organ-on-chip technologies replicate human organ functions, offering a valuable platform for biomarker discovery and validation. These systems simulate physiological environments for disease modeling and drug testing. The organ-on-chip market is expected to grow significantly, reaching $952.4 million by 2030. The FDA is pushing for animal trial reductions in favor of these technologies.
- High-Throughput Screening
Organ-on-chip systems support high-throughput analysis of biomarkers using technologies like PCR, ELISA, and LC-MS. These platforms facilitate drug development and precision medicine advancements. Integration with AI and biosensing accelerates therapeutic discovery.
- Metabolomics for Biomarker Discovery
Metabolomics platforms using nuclear magnetic resonance (NMR) and mass spectrometry analyze comprehensive metabolite profiles, aiding in biomarker discovery. Multivariate data analysis improves accuracy in identifying small metabolites.
These technological advances continue to expand the possibilities for diagnostic biomarker discovery and implementation, making precision medicine more accessible and effective for diverse patient populations.
Despite significant advances in diagnostic biomarker development, several critical challenges continue to limit their widespread clinical implementation and effectiveness.
Challenges and Limitations
The traditional approach to diagnostic biomarker discovery and clinical implementation faces numerous obstacles that slow the translation of research findings into practical healthcare solutions.
- Analytical Variability: Inconsistent results due to different platforms, reagents, and protocols, affecting reproducibility across laboratories.
- Sample Quality and Processing: RNA-based biomarkers are particularly susceptible to degradation during collection, storage, and analysis, impacting stability.
- Complexity of Biological Systems: Confounding factors like age, gender, medications, comorbidities, and circadian rhythms influence biomarker expression, complicating validation.
- High Costs of Development: Substantial financial investments are needed for research, validation, regulatory approval, and clinical infrastructure.
- Cost-Effectiveness Justification: Healthcare systems struggle to justify the cost of biomarker testing, especially when traditional methods remain effective.
- Economic Burden of False Positives: False positives lead to unnecessary follow-up testing, complicating cost-benefit analysis.
- Reimbursement Challenges: Slow reimbursement policies create barriers to adoption, even with clinical evidence supporting biomarker use.
- Regulatory Approval Delays: Complex approval processes for companion diagnostics add time and cost to development.
- Human Biological Variability: Genetic diversity, environmental factors, and population-specific differences can affect biomarker performance across different patient groups.
- Limited Global Applicability: Biomarkers validated in one population may not perform equally well in different ethnic or geographic populations.
- Lack of Standardization: Incomplete standardization of laboratories, platforms, and analytical methods hinders result comparison and meta-analysis.
- Absence of Reference Materials: The lack of standardized reference materials and quality control procedures further complicates the biomarker development process.
The complexity of these challenges has created an urgent need for innovative solutions that can bridge the gap between biomarker discovery and clinical implementation. This is where Biostate AI comes in.
How Biostate AI is Streamlining Disease Prediction and Treatment Challenges
Modern healthcare needs platforms that provide high-quality results while overcoming barriers like cost, accessibility, and complexity. This has led to the creation of integrated platforms that make biomarker research more accessible without sacrificing analytical accuracy.
Biostate AI addresses these challenges with a platform that combines high-quality RNA sequencing and AI-driven analysis. It simplifies the entire process from sample collection to actionable insights, removing traditional barriers while ensuring reliable results.
Key Features:
- Unbeatable Pricing: Get high-quality RNA sequencing starting at just $80 per sample, making comprehensive transcriptomic analysis affordable for large-scale and routine clinical studies.
- Rapid Turnaround: Results are delivered in 1-3 weeks, speeding up biomarker validation and clinical decision-making.
- Complete Transcriptome Insights: Capture both mRNA and non-coding RNA to ensure no potential biomarker is overlooked.
- AI-Driven Analysis: OmicsWeb AI makes complex data interpretation easy, even for researchers and clinicians without bioinformatics expertise.
- Minimal Sample Requirements: Use as little as 10µL of blood, 10ng of RNA, or 1 FFPE slide, maximizing the value of precious clinical samples.
- Low RIN Compatibility: Process RNA samples with RIN values as low as 2, allowing the use of archived or degraded specimens for biomarker discovery.
This approach transforms biomarker development into a streamlined, accessible process, accelerating the shift from molecular insights to clinical applications.
Final Words
The combination of high-throughput sequencing, AI-driven analysis, and cost-effective platforms is making sophisticated diagnostic biomarker tools accessible to more researchers and healthcare providers.
With the diagnostic biomarkers market set to reach hundreds of billions in the next decade, integrating advanced analytical platforms is key to unlocking the full power of precision medicine.
Biostate AI offers a comprehensive platform to help researchers, clinicians, and healthcare organizations turn biological insights into actionable decisions. Our cost-effective AI-driven solution is designed to democratize biomarker research while maintaining the analytical rigor required for clinical applications.
Get in touch to discover how our integrated RNA sequencing and AI analysis capabilities can advance your biomarker research and clinical applications.
FAQs
What makes RNA-based diagnostic biomarkers superior to traditional protein markers?
RNA-based diagnostic biomarkers offer several advantages over traditional protein markers, including their ability to detect disease-related changes earlier in the pathological process, provide dynamic insights into real-time cellular activity, and reveal comprehensive gene expression patterns that single-protein analysis may miss. RNA biomarkers can identify previously unknown disease mechanisms and therapeutic targets while offering higher sensitivity for detecting minimal disease activity or early-stage conditions.
How do machine learning algorithms improve diagnostic biomarker accuracy?
Machine learning algorithms enhance diagnostic biomarker accuracy by analyzing complex, multidimensional datasets that exceed human analytical capabilities. These algorithms can identify subtle patterns in biomarker expression, integrate multiple data types simultaneously, and account for confounding variables that might obscure traditional statistical analysis.
What sample types are most suitable for comprehensive biomarker analysis?
The optimal sample type for biomarker analysis depends on the specific diagnostic application and target disease. Blood samples offer convenience and non-invasive collection while providing access to circulating biomarkers that reflect systemic disease activity. Tissue samples provide the highest concentration of disease-specific biomarkers but require invasive procedures.
How long does it typically take to validate a new diagnostic biomarker for clinical use?
Diagnostic biomarker validation typically requires 3-7 years from initial discovery to clinical implementation, depending on the complexity of the biomarker, regulatory requirements, and clinical validation study design. This timeline includes analytical validation to ensure reproducible and accurate measurements, clinical validation to demonstrate diagnostic performance in relevant patient populations, and regulatory review processes.
