Did you know? The healthcare predictive analytics market will expand from $14.02 billion in 2023 to $126.15 billion by 2032. This represents a compound annual growth rate (CAGR) of 27.67%.
Unlike traditional methods that react to clinical events, predictive modeling in healthcare helps companies anticipate outcomes, spot risks, and make proactive decisions. For pharma and biotech firms, the benefits are clear.
Companies that adopt predictive modeling can speed up drug discovery, cut clinical trial costs, and more accurately target patients. These improvements directly increase trial success rates and shorten regulatory approval times.
This article will explore how predictive modeling delivers tangible value in drug discovery, clinical trials, and patient targeting.
Key Takeaways
- Massive Market Growth: Healthcare predictive analytics will grow from $14.02 billion in 2023 to $126.15 billion by 2032, driven by AI’s ability to reduce drug development timelines from 5 years to 12-18 months.
- Four Key Benefits: Predictive modeling accelerates drug discovery (40% faster target identification), optimizes clinical trials (reduces costs and improves patient selection), enables personalized medicine through genetic analysis, and streamlines operations with demand forecasting.
- Major Implementation Barriers: Organizations struggle with poor data quality, complex system integration, regulatory compliance requirements, talent shortages, and high upfront costs that prevent successful AI adoption.
- Proven Use Cases: Leading companies like Pfizer, Novartis, and Atomwise are already using predictive modeling across drug discovery, clinical trials, and safety monitoring with measurable results, including 89% accuracy in toxicity prediction.
- Accessible Solutions Available: Platforms like Biostate AI eliminate technical barriers by offering complete RNA sequencing and AI analytics starting at $80/sample, making advanced predictive modeling accessible without massive investments or specialized teams.
What is Predictive Modeling in Healthcare?
Predictive modeling in healthcare is the disciplined use of statistical and machine-learning techniques to estimate the probability of future clinical or operational events using curated biomedical, clinicogenomic, and real-world data.
It functions as an end-to-end analytical pipeline that transforms heterogeneous biomedical signals into actionable probability scores that can be embedded into discovery, development, and post-marketing workflows.
Predictive Modeling Workflow
Here is a simplified workflow of predictive modeling:
- Analytical Objective
- Frame a specific biomedical question as a probabilistic forecast, e.g., “Given a compound’s molecular profile, what is the likelihood of cardiotoxicity in first-in-human trials?”
- Data Foundation
- Integrate multi-modal datasets—omics, high-content screening images, electronic health records (EHRs), claims, wearables, digital pathology, and pharmacovigilance feeds—into a common analytical layer.
- Ensure identity resolution across sources to create longitudinal, patient-centric, or molecule-centric feature matrices.
- Algorithmic Engine
- Choose appropriate modeling paradigms: survival models, Bayesian networks, ensemble decision forests, gradient boosting, recurrent neural networks, transformers, or graph neural networks for structure-activity relationships.
- Apply domain-specific constraints (e.g., chemical validity rules, physiologically based PK priors) during learning to preserve biological plausibility.
- Model Training & Evaluation
- Partition development, calibration, and hold-out validation cohorts using time-split or molecule-split strategies to reflect prospective use.
- Measure discrimination (AUROC, AUPRC), calibration (Brier score, calibration slope), and clinical utility thresholds rather than generic accuracy metrics.
- Stress-test with cross-geography and cross-technology external validation to gage transportability.
- Operationalization
- Package the trained model as a versioned container or API; embed within data-science notebooks for discovery teams, eCTD-compliant tools for clinical statisticians, or signal-detection dashboards for pharmacovigilance scientists.
- Monitor model drift via periodic back-testing against fresh RWD and institute automated re-training triggers.
By treating predictive modeling as a validated tool based on biomedical context and regulatory standards, pharma and biotech companies can turn raw, multi-source data into accurate risk and response estimates.
With this structured approach to transforming biomedical data into actionable insights, pharmaceutical companies are now seeing concrete benefits across their entire value chain.
Benefits of Predictive Modeling in Healthcare
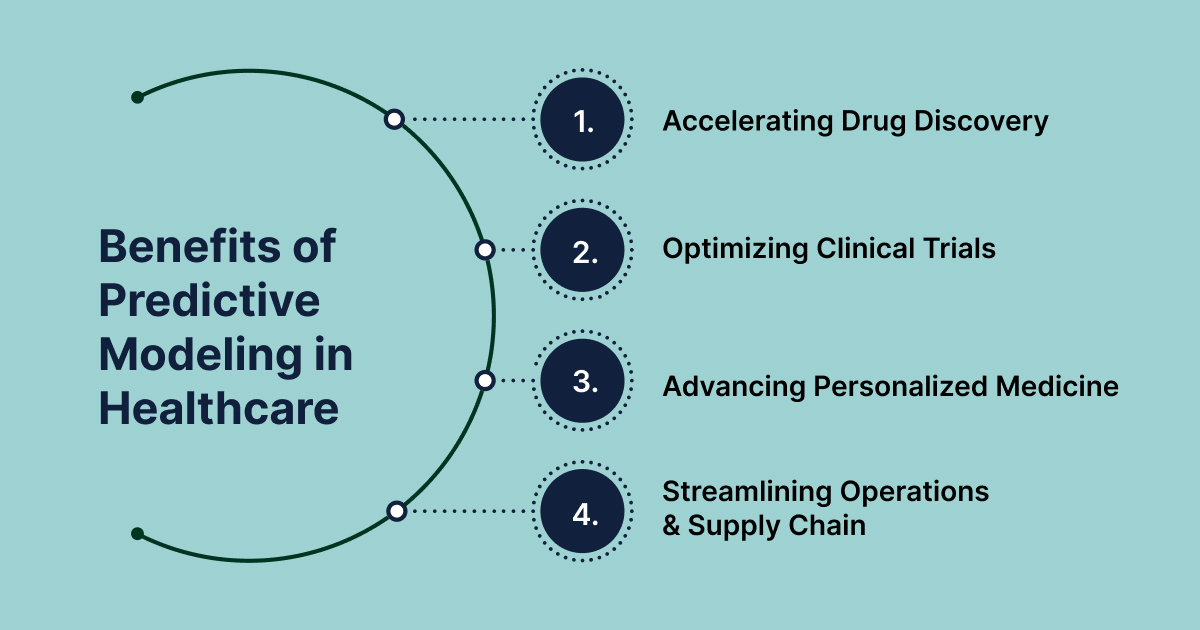
Predictive modeling is fundamentally reshaping the pharmaceutical and biotechnology landscape, delivering tangible benefits across the entire value chain.
1. Accelerating Drug Discovery and Development
Predictive modeling is crucial for speeding up drug discovery and development while cutting costs.
- It can reduce the time spent identifying promising drug candidates by up to 40% and lower costs by 30%.
- AI-driven methods can shorten drug development timelines from five years to just 12-18 months.
- By analyzing large datasets, AI helps identify the best drug candidates earlier, improving the chances of clinical success.
- Machine learning-based virtual screening, for example, is 50 to 100 times more successful than random selection in finding active compounds.
- This shift from traditional trial-and-error methods to more informed, targeted approaches means better resource allocation.
Companies can focus on compounds with higher potential, boosting success rates and reducing costly late-stage failures. This results in a more efficient and profitable R&D pipeline.
2. Optimizing Clinical Trials
Predictive models are changing how clinical trials are conducted by reducing reliance on traditional Randomized Control Trials (RCTs).
- These models use historical data to create virtual patient cohorts, helping to replace animal studies, which may not accurately predict human outcomes.
- They can quickly identify eligible participants, turning what used to be a lengthy process into just a few days.
- This speeds up recruitment, ensures better diversity in trials, and even predicts patient dropouts, preventing costly disruptions.
Predictive analytics also lowers clinical trial costs by improving efficiency.
- It helps with selecting the right candidates, predicting their responses to treatment, and calculating appropriate sample sizes.
- This proactive approach addresses issues before they arise, improving trial validity and giving companies a competitive edge.
- For example, Pfizer used predictive analytics to speed up its COVID-19 vaccine trial, cutting the timeline to under a year.
By using these models, companies can reduce the number of participants, focus on the right groups, and boost trial success rates, all while minimizing costs and speeding up time to market.
3. Advancing Personalized Medicine and Patient Outcomes
Predictive analytics helps pharmaceutical companies predict how a drug will perform in specific patient groups before large-scale clinical trials begin. This is crucial for personalized medicine, allowing treatments to be tailored to individual needs.
Predictive models can identify genetic variations linked to disease risk and drug response.
- For example, polygenic risk scores (PRS) combine multiple genetic factors to predict the risk of developing certain diseases.
- Predictive analytics also helps with drug safety, identifying patients at risk of adverse drug reactions (ADRs) by analyzing clinical trial data and electronic health records.
These models can even simulate treatment effects when clinical trials are too costly.
- Novartis, for example, uses predictive analytics and genomic data to improve personalized oncology treatments, like Kisqali for HER2-positive breast cancer.
- By integrating data from patient characteristics, genomic profiles, and real-world outcomes, predictive models create a fuller understanding of patient responses.
This leads to safer, more effective treatments.
4. Streamlining Operations & Supply Chain Management
Predictive modeling plays a key role in optimizing pharmaceutical operations and supply chain management.
- It helps companies forecast demand spikes and spot potential disruptions before they happen. In manufacturing, AI-driven systems reduce errors and improve product consistency, making production more efficient.
- Real-time analytics allow production lines to adjust quickly, improving both quality and speed.
- A crucial application is predictive maintenance, which uses sensor data to identify equipment issues before they cause problems.
- This prevents downtime and keeps production running smoothly. It also ensures production schedules stay on track, avoiding delays that could affect drug availability.
- During the COVID-19 pandemic, Pfizer used predictive analytics to forecast vaccine demand, ensuring efficient production and preventing shortages.
These broad benefits become even more compelling when we examine specific applications where predictive modeling is already delivering measurable results.
Use Cases of Predictive Modeling in Healthcare
Predictive modeling is being applied across every stage of the drug lifecycle, from initial discovery to commercialization, driving innovation and efficiency.
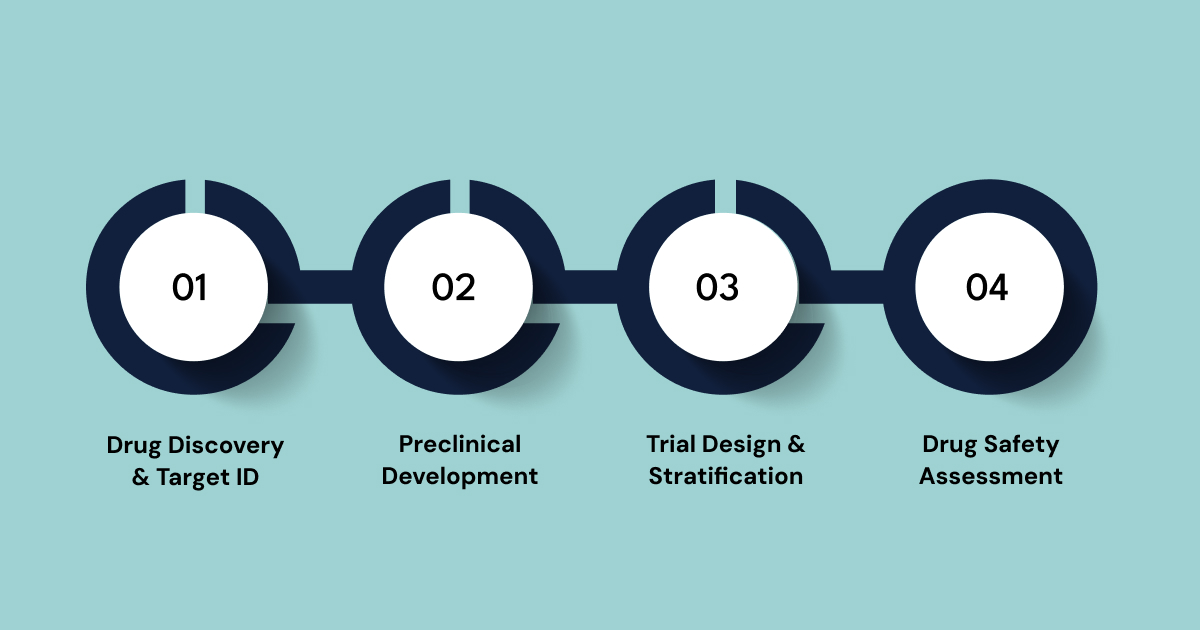
1. Early Drug Discovery & Target Identification
Generative AI is transforming drug discovery by predicting how potential treatments will interact with protein targets. This speeds up the process and allows for treatments tailored to specific needs.
- Atomwise, a preclinical pharmaceutical research company, uses AI to find “undruggable targets.” Their technology, AtomNet®, has outperformed other AI platforms and is used by over 250 life science organizations worldwide. In 2022, Atomwise secured a $1.2 billion deal with Sanofi to develop small molecules.
- Insilico Medicine also uses generative AI to discover new drug molecules and predict their clinical outcomes. One of their compounds, ISM5411, is a groundbreaking potential treatment for Inflammatory Bowel Disease (IBD) that doesn’t rely on immunosuppression. It entered Phase I trials in early 2024 and received positive results.
- NEBULA, a French startup using AI to map the 3D structure of macromolecules.
- Silica Corpora is a German startup designing therapeutic antibodies with AI-powered protein models.
These advances highlight how generative AI is speeding up drug discovery and opening new treatment possibilities.
2. Preclinical Development & Lead Optimization
Predictive modeling is transforming preclinical development by simulating drug behavior before physical testing on animals or humans. This stage benefits from several cutting-edge technologies:
- Organ-on-a-Chip and Microphysiological Systems: These dynamic platforms simulate human organs, cells, and tissues on microfluidic chips, mimicking biological reactions more effectively than traditional cell cultures or animal models. Highlights from recent summits include heart and liver-on-chip for early toxicity diagnosis, coupled with AI-driven image analysis and whole-body pharmacokinetics.
- 3D Bioprinting & Advanced Cell Models: Researchers are now using 3D or 2D printed tissue models to more precisely replicate the human cellular environment. This includes co-culture systems that use the immune tumor microenvironment and scaffold-free printing to create neural, lung, or liver tissues, providing better translation and improved screening results.
- Digital Twins in Preclinical Simulation: Digital twin tools are increasingly used to model patient avatars and virtual organs, simulating drug interactions to understand dose response. These tools merge in silico modeling with in vitro data to create hybrid systems, allowing for virtual preclinical testing.
- CRISPR & Gene Editing: Beyond a gene-editing tool, CRISPR is a full-fledged research engine identifying specific patient mutations for special therapies and functional genomes for new therapeutic targets.
- High-Throughput Screening Platforms: These platforms offer scale and speed with automated robotics, multiplex assay integration, and real-time data analysis, enabling early-stage screening of compounds and checking drug interactions in real time.
3. Clinical Trial Design and Patient Stratification
Predictive models help companies reduce the number of test subjects, ensuring only suitable groups are included. This boosts trial success rates, minimizes waste, speeds up time to market, and cuts costs.
Leading solutions exemplify these capabilities:
- Medidata AI’s “Intelligent Trials” leverages the industry’s largest clinical trial dataset to provide predictive analytics for enrollment, forecasting recruitment rates, and flagging underperforming sites. It also assists in protocol design optimization and can simulate trials to guide feasibility and design choices.
- Launch Therapeutics, a biotech consortium, used Medidata’s platform to rank investigators and sites based on AI-driven performance predictions for late-stage trials.
- Oracle Clinical One embeds AI features to improve patient matching and site selection, predicting which study sites are likely to enroll patients fastest.
- Saama Technologies’ Life Science Analytics Cloud (LSAC) includes modules for AI-based patient recruitment, protocol design analytics, and risk-based trial monitoring. This is capable of predicting patient dropout rates or underperforming sites.
- A top-5 pharma company used Saama’s AI to reduce trial protocol amendments, saving time, and Pfizer partnered with Saama in 2022 for several trials.
- Trial Pathfinder, an open-sourced AI framework from Stanford University, allows life science organizations to access real-world patient health records to simulate drug trials, evaluate drug efficacy, and survival ratios. It was notably used to evaluate over 61,000 patients for eligibility in a non-small-cell lung cancer oncology trial.
- Amgen’s Analytical Trial Optimization Module (ATOMIC) analyzes extensive data to identify high-potential clinical trial sites that can enroll patients quickly, shifting from reactive to proactive planning.
Also, AI and ML help discover biomarkers and predict treatment responses, with deep learning algorithms achieving accuracy rates over 85%. Polygenic risk scores (PRS) predict disease risk by combining genetic variants.
4. Pharmacovigilance & Drug Safety Assessment
Predictive analytics is highly effective for drug safety assessment and identifying specific patient groups at risk of adverse drug reactions (ADRs).
For instance, PharmBERT has demonstrated superior performance in tasks such as adverse drug reaction detection and ADME (absorption, distribution, metabolism, and excretion) classification. This proactive identification of potential safety concerns allows for earlier intervention and risk mitigation, enhancing patient safety post-market.
Predictive modeling improves manufacturing by reducing errors and enhancing consistency with AI-driven real-time analytics. Predictive maintenance prevents machine failures, maximizing efficiency and uptime. Digital twins simulate production schedules, ensuring smooth operations and avoiding disruptions that could affect drug availability.
While these success stories demonstrate predictive modeling’s potential, the path to implementation is not without obstacles that organizations must carefully navigate.
Implementation Challenges of Predictive Modeling
We often face several challenges while implementing predictive modeling. These challenges span data, regulatory, ethical, human capital, and scalability dimensions.
The following tables summarize these challenges and the regulatory landscape:
| Challenge | Description | Mitigation Strategy |
| Data Quality & Integrity | Inconsistent, incomplete, or inaccurate data leading to erroneous predictions, poor product quality, and regulatory violations. | Implement robust data cleaning, continuous data quality assessments, and standardized data collection protocols. Invest in scalable data platforms (e.g., Apache Kafka, MongoDB). |
| System Integration | Difficulty integrating new AI/IoT solutions with existing legacy systems, leading to time-consuming and costly processes. | Proactive investment in upgrading legacy systemsPrioritize compatibility; adopt modular system architectures. |
| Regulatory Compliance | Navigating evolving and complex FDA/EMA guidelines for AI/MLEnsuring model trustworthiness, transparency, and validation. | Engage early with regulatory bodiesDevelop risk-based credibility assessment plansEnsure detailed model documentation and validation. |
| Ethical Concerns & Bias | Algorithmic bias from non-representative training dataLack of explainability (“black-box” models)Patient privacy risks. | Use diverse, inclusive datasetsConduct regular bias auditsImplement Explainable AI (XAI) methodsAdopt strong encryption and access controls (HIPAA/GDPR compliance). |
| Talent & Data Literacy Gaps | Scarcity of experts (data scientists, statisticians)Lack of data literacy within departmentsOrganizational resistance to change. | Invest in upskilling programsFoster a culture of AI literacy and data-driven decision-makingSeek strategic partnerships for specialized expertise. |
| Scalability & Investment | Difficulty scaling pilot projects to large-scale operationsSignificant upfront investment in technology and human resources. | Careful planning for scalable architecturesModular system designExplore partnerships with technology providersDemonstrate clear ROI for investment justification. |
Fortunately, these implementation barriers are not insurmountable when organizations have access to the right tools and partnerships like what Biostate AI offers.
How Biostate AI Can Streamline Predictive Modeling in Healthcare
Organizations face major hurdles when implementing predictive modeling in healthcare. These challenges often prevent companies from realizing the full potential of AI-driven insights in drug discovery and patient care.
Biostate AI addresses these barriers with an integrated platform that combines high-quality RNA sequencing, automated analytics, and proven AI models. Our solution transforms raw biological samples into reliable predictive insights while eliminating the technical complexities that typically slow down implementation.
Key features that solve implementation challenges:
- Complete Data Quality Control: Total RNA sequencing covers both mRNA and non-coding RNA, ensuring comprehensive datasets. Works with minimal samples (10µL blood, 10ng RNA) and low-quality RNA (RIN as low as 2).
- Unified Platform Integration: OmicsWeb eliminates fragmented workflows by combining data storage, analysis, and visualization in one system. Supports multiple data types: RNA-Seq, WGS, methylation, and single-cell.
- No-Code Analytics: AI Copilot allows natural language queries, removing the need for specialized programming skills. Automated pipelines deliver publication-ready results without manual intervention.
- Regulatory-Ready Documentation: Biobase foundational model provides transparent, validated algorithms with proven performance metrics (89% accuracy in drug toxicity prediction, 70% accuracy in AML therapy selection).
- Cost-Effective Scaling: High-quality sequencing starts at $80/sample with 1-3 week turnaround times. Flexible sample processing accommodates various research needs and timelines.
- Expert Partnership Model: Complete service handling from sample collection to final insights reduces the need for in-house technical expertise while maintaining full control over research objectives.
This comprehensive approach transforms predictive modeling from a complex technical challenge into a streamlined, accessible process that organizations can implement regardless of their current infrastructure or expertise levels.
Final Words
Predictive modeling in healthcare accelerates drug discovery by analyzing data more efficiently. It optimizes clinical trials by improving patient selection and monitoring. Personalized medicine benefits from tailored treatment plans based on predictive insights. These advances reduce development timelines from five years to 12-18 months and cut costs by up to 30%. Despite these benefits, companies face challenges such as poor data quality, complex system integration, and navigating regulatory requirements.
Biostate AI helps you overcome these barriers with a comprehensive RNA sequencing and analytics platform starting at just $80 per sample. Our solution handles everything from sample processing to final insights, making predictive modeling accessible without large upfront costs or specialized teams.
Transform your research with cost-effective predictive modeling. Contact us today to accelerate your drug discovery and development programs.
FAQs
1. How long does it typically take to see ROI from predictive modeling investments in healthcare?
Most pharmaceutical companies begin seeing returns within 12-18 months of implementation. Early wins often come from improved patient recruitment efficiency and reduced protocol amendments in clinical trials. Full ROI typically materializes within 2-3 years as companies optimize drug discovery processes and reduce late-stage development failures.
2. What data security measures are essential when implementing predictive modeling with patient information?
Healthcare predictive modeling requires HIPAA compliance, end-to-end encryption, and secure data anonymization protocols. Organizations must implement role-based access controls, regular security audits, and ensure all third-party platforms meet healthcare data protection standards. Cloud-based solutions should offer dedicated healthcare instances with additional security layers.
3. Can predictive modeling work effectively with small datasets, or do you need massive amounts of data?
While larger datasets generally improve model accuracy, modern techniques like transfer learning and domain adaptation allow effective modeling with smaller, high-quality datasets. For specialized rare diseases or novel targets, predictive models can leverage pre-trained foundations on related biological data. The key is data quality and relevance rather than just volume.
4. How do regulatory agencies like FDA view AI-generated predictions in drug development submissions?
The FDA has published guidance on AI/ML in drug development, emphasizing the need for model transparency, validation, and clear documentation of training data and performance metrics. Regulatory bodies are increasingly accepting AI-generated evidence when accompanied by proper validation studies and clear explanations of model limitations and decision boundaries.
